30, Jan 2024
Navigating The Landscape Of Prior Authorization In Oregon: A Comprehensive Guide To D-MAP Forms
Navigating the Landscape of Prior Authorization in Oregon: A Comprehensive Guide to D-MAP Forms
Related Articles: Navigating the Landscape of Prior Authorization in Oregon: A Comprehensive Guide to D-MAP Forms
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Navigating the Landscape of Prior Authorization in Oregon: A Comprehensive Guide to D-MAP Forms. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Landscape of Prior Authorization in Oregon: A Comprehensive Guide to D-MAP Forms
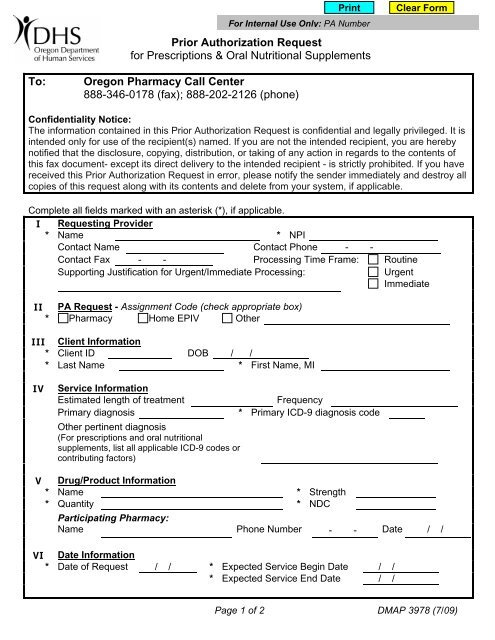
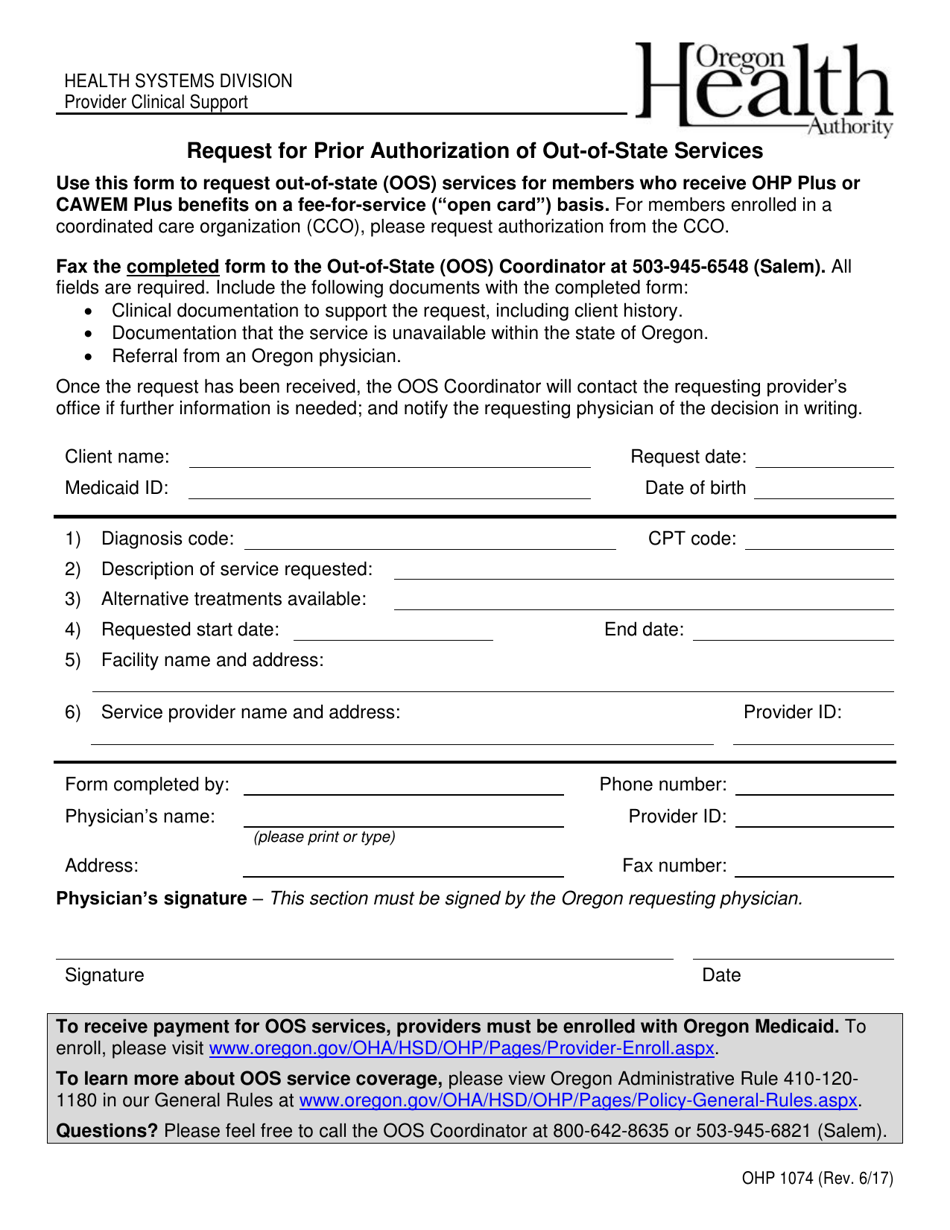
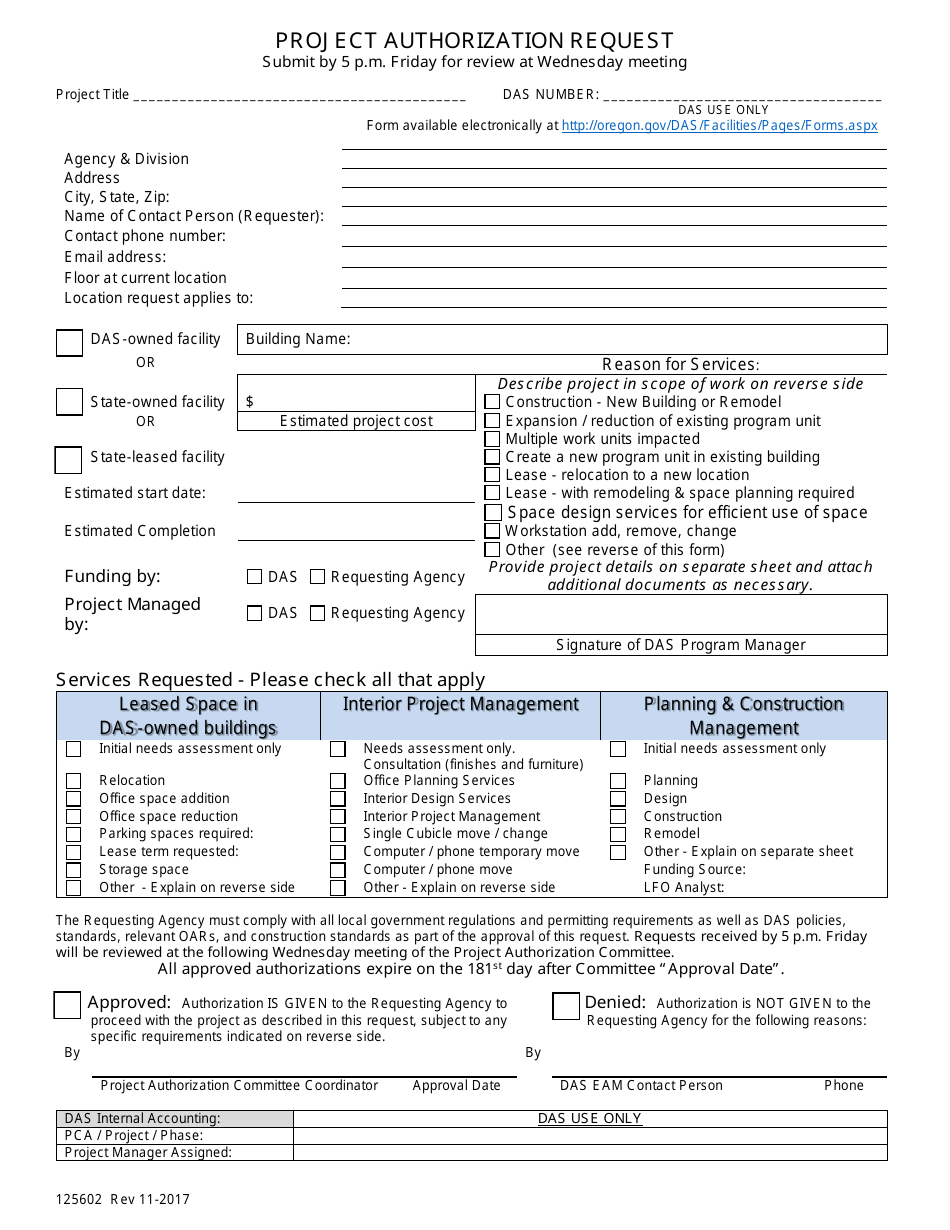
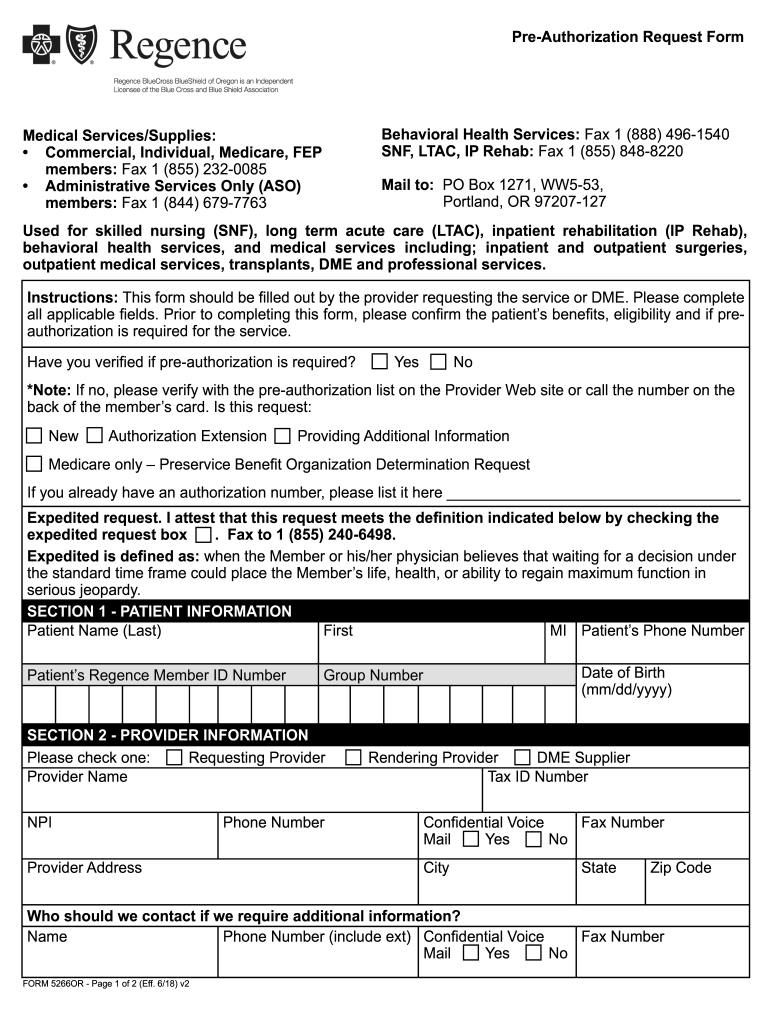
The healthcare landscape is intricate, often demanding a complex interplay of procedures and documentation. One such aspect, often encountered by patients and providers alike, is the process of prior authorization. This process, a crucial element of healthcare cost containment and ensuring appropriate medical care, requires healthcare providers to obtain approval from the patient’s insurance plan before specific treatments or medications can be administered. In Oregon, this process is streamlined through the D-MAP (Drug Management Assistance Program) forms.
Understanding D-MAP Forms: A Foundation for Effective Healthcare Delivery
D-MAP forms are a standardized tool for healthcare providers in Oregon, serving as a vital communication bridge between providers, patients, and insurance companies. These forms are designed to facilitate the prior authorization process for medications, ensuring that prescribed treatments are medically necessary, cost-effective, and aligned with the patient’s individual needs.
Key Elements of D-MAP Forms:
- Patient Information: D-MAP forms require the patient’s personal details, including name, date of birth, insurance information, and medical history.
- Medication Request: The form details the requested medication, including its name, dosage, frequency, and duration of treatment.
- Clinical Justification: The provider must provide a comprehensive rationale for the medication request, outlining the patient’s diagnosis, treatment goals, and why the chosen medication is the most appropriate option.
- Alternative Treatments: The form necessitates documentation of alternative treatments considered and the reasons for choosing the requested medication over these alternatives.
- Patient’s Current Medications: A complete list of the patient’s existing medications, including their dosages and frequencies, is required.
- Provider Information: The form includes details about the prescribing provider, including their name, contact information, and medical license number.
The Importance of D-MAP Forms: Ensuring Quality and Efficiency
D-MAP forms are not just a bureaucratic hurdle; they play a critical role in enhancing the quality and efficiency of healthcare delivery in Oregon. By standardizing the prior authorization process, D-MAP forms:
- Streamline Communication: They create a clear and concise channel of communication between providers, patients, and insurance companies, minimizing misunderstandings and delays.
- Enhance Patient Safety: By requiring providers to justify their medication choices, D-MAP forms ensure that prescribed treatments are clinically appropriate and safe for the patient.
- Promote Cost-Effectiveness: The forms encourage providers to consider cost-effective alternatives and prioritize treatments that offer the best value for patients and insurers.
- Reduce Administrative Burden: The standardized format of D-MAP forms simplifies the process for providers, reducing the administrative burden associated with prior authorization requests.
Navigating the Process: A Step-by-Step Guide
- Identify the Need for Prior Authorization: Providers must first determine whether the requested medication requires prior authorization based on the patient’s insurance plan guidelines.
- Complete the D-MAP Form: Providers must accurately and thoroughly complete all sections of the form, including the patient’s information, medication request, clinical justification, and alternative treatment considerations.
- Submit the Form: The completed form can be submitted electronically through the insurance company’s online portal or by fax or mail, depending on the specific insurance plan’s instructions.
- Processing and Review: Insurance companies review the submitted D-MAP form, assessing the medical necessity of the requested medication and its alignment with the patient’s insurance plan coverage.
- Decision and Communication: The insurance company communicates its decision regarding the prior authorization request to the provider and the patient. If approved, the medication can be dispensed and administered.
Frequently Asked Questions (FAQs) Regarding D-MAP Forms
Q1: Who is responsible for completing D-MAP forms?
A: The prescribing provider is responsible for completing and submitting D-MAP forms for prior authorization requests.
Q2: What happens if a D-MAP form is incomplete or inaccurate?
A: Incomplete or inaccurate D-MAP forms may result in delays in processing the prior authorization request. The insurance company may request additional information or clarification before making a decision.
Q3: What if a prior authorization request is denied?
A: If a prior authorization request is denied, the provider can appeal the decision by submitting additional supporting documentation to the insurance company.
Q4: Are there resources available to help providers complete D-MAP forms?
A: Yes, many insurance companies offer online resources, FAQs, and dedicated support teams to assist providers in completing D-MAP forms accurately and efficiently.
Q5: Are there specific timeframes for processing D-MAP forms?
A: The processing timeframe for D-MAP forms varies depending on the insurance company and the complexity of the request. However, most insurance companies strive to process requests within a reasonable timeframe.
Tips for Successful D-MAP Form Completion:
- Thorough Documentation: Ensure all sections of the form are completed accurately and comprehensively, providing detailed clinical justification for the medication request.
- Clear and Concise Language: Use clear and concise language, avoiding medical jargon that may not be understood by the insurance company reviewers.
- Supporting Documentation: Include any relevant supporting documentation, such as medical records, test results, or prior treatment history, to strengthen the request.
- Timely Submission: Submit the completed form well in advance of the expected start date of the medication to allow sufficient time for processing.
- Follow-Up: If there are delays or if the status of the request is unclear, follow up with the insurance company to ensure timely processing.
Conclusion: A Foundation for Efficient and Effective Healthcare Delivery
D-MAP forms are a crucial element of the prior authorization process in Oregon, ensuring that prescribed treatments are medically necessary, cost-effective, and aligned with patient needs. By streamlining communication, enhancing patient safety, and promoting cost-effectiveness, D-MAP forms contribute significantly to the overall efficiency and effectiveness of healthcare delivery in the state.




Closure
Thus, we hope this article has provided valuable insights into Navigating the Landscape of Prior Authorization in Oregon: A Comprehensive Guide to D-MAP Forms. We appreciate your attention to our article. See you in our next article!
- 0
- By admin
